New neurons against stress
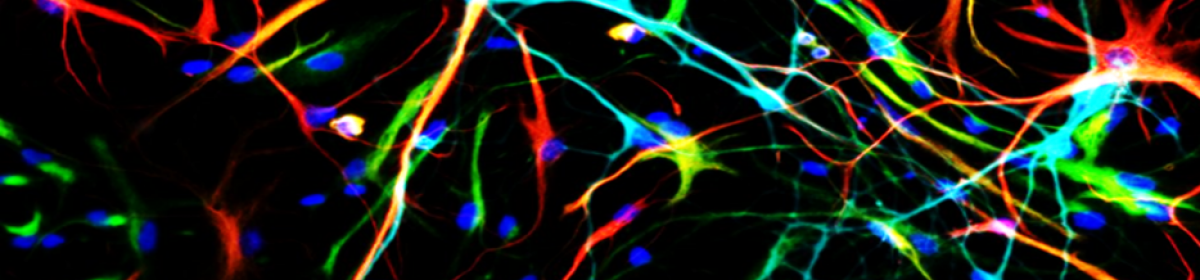
One of the nicest papers this month came out of the lab of René Hen, published in Nature. They looked at adult hippocampal neurogenesis (AHN). This is the birth of new neurons in the adult brain, specifically in the hippocampus. The fact that this happens has been known for some time, but there has been a lot of debate about what these cells do. People have shown they play a role in things like pattern separation, spatial navigation, and certain forms of memory.
Now Anacker et al show – using some really cool techniques – that these new neurons play a crucial role in the response to stress. They used a technique called DREADD, which sounds more ominous than it is. These are engineered protein receptors, which don’t respond to any natural substances. If you put these receptors in the neurons of a mouse, you can turn them on or off whenever you want to, just by giving the animal the appropriate drug that the artificial receptor responds to. This is a really powerful technique, as you can study what these neurons do during behavioural testing.
What Anecker et al did was to subject mice to mild stress, that doesn’t have much of an effect in normal animals. However, when they used DREADDs to selectively switch off the activity of newly born neurons, the animals responded as if they’d had a much more severe stress. Using genetic tricks to increase the number of newly born adult neurons had the opposite effects; animals responded much less to stress.
There is a lot more work in this paper, showing part of the mechanism of this, but the take home message is that these adult born neurons seem very important for making sure there is no over-response to stress. Interestingly, stress is also one of the things well known to decrease adult neurogenesis. This might be a mechanism by which chronic stress can have such profoundly negative effects. Initially there are plenty of adult born neurons there to help modulate the stress response, but later on, as the stress is starting to decrease the number of new neurons, this modulation decreases, and the negetive effects start becoming more and more pronounced.
All of this will be hard to prove in humans, but food for thought nonetheless!
Another link between the immune system and schizophrenia
Those of you who have read my previous work know I’m very interested in the link between the immune system and psychiatric diseases – in fact, it’s what my employer pays me to be interested in. This month a new analysis came out in Biological Psychiatry about the link between auto-immune diseases in psychosis (good overview by the author here)
A link between the immune system and schizophrenia has been talked about for decades. The first evidence was that infection of a mother during pregnancy increases the risk for her child to get schizophrenia later in life. Work in models suggests this probably isn’t actually due to the infection itself, but due to the immune response of the mother affecting the development of the foetus.
This new paper, a meta-analysis taking together decades of other studies, now shows that people suffering from a range of auto-immune diseases have an increased risk of also suffering from psychosis, a prominent symptom of schizophrenia and some other disorders. Auto-immune diseases, where the immune system mistaking starts attacking some of your own proteins, leads to long-term activation of the immune system. The ones found to be associated with psychosis in this paper are (in order of risk) pemphigoid, pernicious anaemia, psoriasis, coeliac disease, and Graves’ disease.
What does this tell us? It seems that chronic immune activation is a risk factor for developing psychosis. This fits in with the fact that those suffering from schizophrenia have been shown to have higher levels of inflammatory molecules in their system.
The really interesting point is that not all diseases are associated with psychosis. In fact, two of them – rheumatoid arthritis and ankylosing spondylitis are the opposite, they are associated with a lower risk. We don’t know if that’s because the diseases are different, or the treatments used for them are somehow protective. Interestingly both of these diseases are commonly treated with drug that neutralise a pro-inflammatory protein called TNFα. Might be a mechanism there….
Not all microglia are created equal
Ah microglia. No, I won’t stop going on about them! Why not? Because they are very important! Over the last few years we’ve moved far beyond just thinking about them as the “immune cells of the brain”. Yes, microglia are responsible for detecting and clearing out infections in the brain, but they do a lot more than that. They help shape neuronal connections, and modify neuronal activity. One of their other important jobs is to clear up dead cells and cell debris.
In a paper by Ayata et al in Nature Neuroscience (News & Views summary here) we learn more about this last function. They start by looking at two different populations of microglia from different brain areas, the striatum and the cerebellum. The striatum has low levels of cell death (and thus clearance requirements), whereas the cerebellum has higher levels.
They found that microglia isolated from the cerebellum are much better at clearing dying cells than those from the striatum, and that these cells also expressed different genes to those which are worse at cell clearing. Using some clever techniques, they were able to show a specific protein complex called PRC2 controls microglia clearance ability.
This is all interesting (to me at least), but why should we care? The authors answer that question as well. Using mice that didn’t have crucial protein in the PRC2 complex, they showed that microglia clearance is increased. This might sounds like a good thing, being better at taking out the trash. However, the microglia starting clearing things that shouldn’t have been cleared. This included removing perfectly functional neuronal connections, something that led to all sorts of behavioural abnormalities and a tendency to develop epilepsy.
This may be an interesting model for what happens when microglia go wrong. Excessive removal of neurons connection by microglia is thought by some to be part of diseases such as Alzhmier’s and schizophrenia. This work shows us one potential mechanism how that could happen.
Rock out! Modifying brain function with sound
Us neurobiologists are never happy with just observing cell and animals. We want to mess around with things, to see how they work. However, that’s easier said than done. The problem is that the brain is protected by the blood-brain-barrier (BBB). This is a complex system of cells and structures that separates the brain from the rest of the body. Basically, something will only get into the brain if the BBB allows it. And it’s fussy.
Say you want to use DREADDs, as in the first paper described above, to study neurons. You get those into the neurons with a virus. However, if you just inject the mouse with the virus, the BBB will never let it in, and it doesn’t reach the brain. So we have to be bracingly direct. We drill a hole in the animal’s skull, and inject the virus directly into the brain. It works, but it’s not ideal. Now there’s a paper in Nature Biomedical Engineering which does it differently.
Szablowski et al use a technique that’s been in development for a while, the use of ultrasonic sound to temporarily disrupt the blood-brain-barrier. You’ll be familiar with ultrasonic sound from baby ultrasounds. However, if you turn the dial up to 11, you can do a lot more with it. They injected animals with DREADD carrying viruses and a dose of microbubbles. Once these were distributed throughout the circulation, the brains of the animals were stimulated with ultrasound.
To minimise the brain area exposed to the ultrasound, they used eight sources on the outside of the skull. Each individual beam of ultrasound didn’t do anything, but where the eight beams intersected, the desired effect was seen. The use of intersecting beams also allowed them to target specific brain areas, by moving the point of intersection. At the focus of the ultrasound, the microbubbles start expanding and collapsing, which somehow opens up the BBB there for a few hours, allowing the virus to get in.
Long story short: it worked. The authors show that the virus got into the brain, infected the neurons, and allowed them to alter the behaviour of the animals through the DREADDs delivered, without doing any major damage to the brain tissue. This could potentially be a very useful technique, replacing invasive surgery.
Stay tuned for more posts here on Neuroscience Ramblings, and in the mean time, follow me on Twitter: @DrNielsHaan
One thought on “What’s new? – July 2018”