You can find out latest preprint, “Haploinsufficiency of the schizophrenia risk gene Cyfip1 causes abnormal postnatal hippocampal neurogenesis through a novel microglia dependent mechanism” here. This work, which I did most, but certainly not all the work for, links three very different areas of research together, areas which have not been linked before. These are adult neurogenesis, genetic risk for schizophrenia (and other psychiatric diseases), and microglia.
Most of the brain can’t make any new cells in adulthood. However, the hippocampus is an exception to this rule. Here, in a structure called the subgranular zone of the dentate gyrus sit neural stem cells, which can make new neurons throughout life in a process called adult hippocampal neurogenesis. These adult born neurons are specifically used in several functions of the hippocampus, mostly to do with memory. Interestingly, there is some evidence hippocampal neurogenesis is disrupted is psychiatric patients, including in schizophrenia, and might be involved in some of the symptoms of these diseases.
Making new neurons in the adult brain broadly requires four phases. The first is cell division. This is when the stem cells that sit in the subgranular zone divide to generate new cells that will eventually become neurons. The second phase is differentiation. This is when a cells slowly change from a stem cell to something that will become a neuron. Call it neuronal puberty. In parallel with this, the third phase starts, which is cell migration. The developing neurons move from their birthplace into the adjacent granular zone to their eventual final location. This is where the last phase takes place, which is maturation. This is when the new neuron wires into the exiting circuitry and starts functioning. In rodents, this process takes up to eight weeks.
As a lab, we use a lot of genetic models of schizophrenia. Now, I’ve written about schizophrenia models before, so I’m not going to go on about their validity. What we used here was a mouse model for a human genetic risk factor called the 15q11.2(BP1-BP2) CNV. This means carriers have a small deletion in one copy of chromosome 15. Carrying this deletion doubles your risk for schizophrenia, as well as increasing risk for autism, epilepsy, and developmental delay amongst other things. One of the genes in this deletion is called Cyfip1. This gene is interesting because it has previously been shown to affect neuronal connectivity. For this and other reasons, we used a mouse model, which lacks one of the two copies of Cyfip1. In this mouse, we looked at adult hippocampal neurogenesis.
We looked at all phases of neurogenesis in these mice. We showed that there is no effect of the mutation on the rate of cell division, or the birth of the new neurons, either in the brain or when we grow the stem cells in a dish. However, what we do see in both conditions are larger numbers of immature neurons, which are in the process of differentiating, again both in the brain and in the dish. This difference stays when you look later on when the cells have migrated to their final positions and have matured.
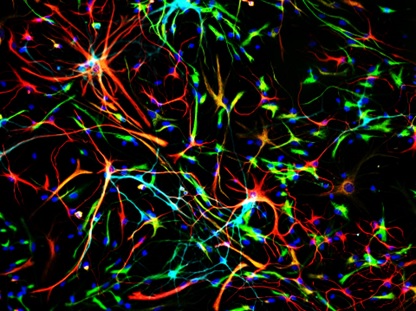
If more neurons aren’t being made, but you’re still seeing more neurons at the end, there is one obvious way to do this, that is to have more of them survive. In normal neurogenesis, well over half of all potential neurons die during the maturation process. If fewer die, you would end up with more neurons without having to make more at the start. Turns out this is exactly what is happening in our mice missing a copy of Cyfip1. Both in a dish and in the brain, there are fewer immature neurons dying.
Now, it was known that this cell death happens, but what causes it wasn’t well known yet. For this we looked at micorglia, the immune cells in the brain. These cells turn out to regulate many things in the brain, as I’ve talked about before here and here. We wondered if they could be the cells regulating the death of these new born neurons. First we looked at whether this was the case. Turns out that if you take out microglia from growing stem cells isolated from mouse brain, neurons survive better, and vice versa if you add more microglia, new neurons die more. So yes, microglia do regulated the survival of neurons at this stage.
So is this the mechanism through which loss of one copy of Cyfip1 affects neuronal survival? To start to work this out, we looked at the effects of the mutation on the functioning of microglia. Although microglia do make Cyfip1 (which nobody knew to start with), and their activation may be somewhat affected, overall the mutated microglia were pretty normal.
So are microglia not to blame? No, they are! The last set of experiments I did shows this clearly. If you grow cells in a dish, you do this in a nutrient solution called medium. While the cells are growing in this, the secret all sorts of factors into the media. Turns out that if you put medium in which microglia have grown on stem cell cultures, this can still cause the death of the new neurons (this is called a conditioned medium experiment). However, what happens when you put on medium in which Cyfip1 mutant microglia have grown on the stem cells? Nothing. Nada. Absolutely zilch.
So what do these results tell us? It tells us that in the normal situation, microglia regulate the numbers of adult born neurons by inducing cell death in some of them, which we didn’t know before. In the Cyfip1 mutant animals, microglia have somehow lost this ability, which means we get more surviving neurons than normal. (If you’re with me so far and have thought this through there could be another possibly, Cyfip1 mutant neurons can’t react to the signals from microglia. I tested this, and they can do this just fine. So it’s definitely the microglia)
Of course, there are still plenty of remaining questions. What do these excess neurons actually do in the brain? How exactly do microglia cause cell death in immature neurons? What does Cyfip1 actually do in microglia? We’re working hard on answering those questions right now, so all I can say have patience and you’ll hear about it here first.
Stay tuned for more posts here on Neuroscience Ramblings, and in the mean time, follow me on Twitter: @DrNielsHaan
PS: There seems to be something going on with cell migration in these animals as well, but you’ll have to wait for the next preprint to hear about that….